March 11, 2016 // Obstructive Sleep Apnea: Know the Signs, Take Action
The National Sleep Foundation’s Sleep Awareness Week is March 6-12. In honor, this article raises awareness about obstructive sleep apnea (OSA), a sleep disorder. Stay Fully Charged and ahead of OSA by learning about the signs/symptoms, diagnosis, and treatment options discussed in this article and its source materials.
Has your ability to concentrate or remember details gotten a little worse over time? Do you get irritated or distracted more easily than you used to? Does your spouse tell you that you snore loudly, stop breathing, or gasp during your sleep? If you have experienced any of these, it’s possible that you have obstructive sleep apnea, or OSA.
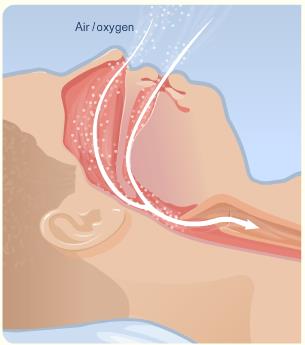
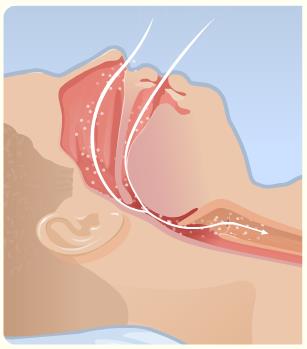
According to the National Heart, Lung, and Blood Institute (NHLBI), OSA is a sleep-related breathing disorder in which your diaphragm continues to try pulling air into your lungs during sleep, but the muscles in your throat relax and partly or completely block the flow of air into your lungs:
Normal flow of air and oxygen into lungs.
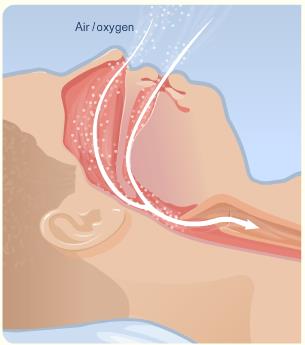
Partly blocked flow of air and oxygen into lungs.
Completely blocked flow of air and oxygen into lungs.
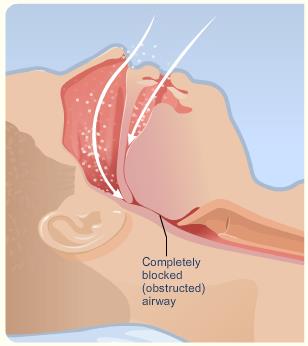
Images: National Heart, Lung, and Blood Institute
Some Symptoms of OSA:
- Difficulty concentrating or remembering, cloudy thinking;
- Irritability, distractibility;
- Struggling to stay awake during meetings, while watching TV at home;
- Spouse tells you that you snore loudly, stop breathing, or gasp during your sleep.
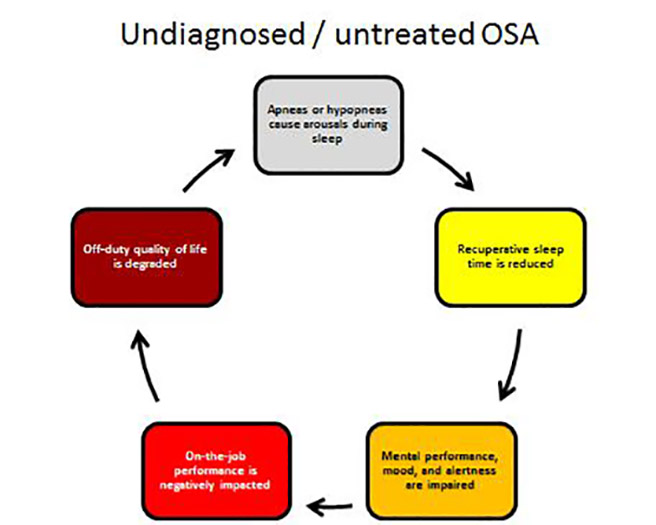
In the United States, the American Academy of Sleep Medicine (AASM) sets standards for diagnosis and treatment of sleep disorders. The AASM states that OSA “…occurs when the muscles relax during sleep, causing soft tissue in the back of the throat to collapse and block the upper airway. This leads to partial reductions (hypopneas) and complete pauses (apneas) in breathing that last at least 10 seconds during sleep.”
The apneas and hypopneas that characterize OSA trigger very brief awakenings during sleep. These occur repeatedly throughout your sleep period (whether at night or during the day) – and often are not remembered. Awakenings impair recuperation during sleep – effectively leading to a sleep debt. Even if you devote seven to eight hours trying to sleep, if you have OSA, the amount of recuperative sleep you actually obtain can be much less than seven-to-eight hours.
This sleep debt causes the mental impairments listed above. These impairments often are subtle and you may not be aware of them, especially if they have increased slowly over months or years. More obvious – but not always present – is excessive sleepiness during waking hours, with individuals struggling to stay awake on the job or while driving.
How widespread is OSA?
According to AASM, results from early studies indicated that approximately 24 percent of men and 9 percent of women showed breathing symptoms of OSA, even if they did not experience daytime sleepiness. Results from those early studies also indicated that OSA severe enough to cause daytime sleepiness only occurred in 4 percent of men and 2 percent of women. But with the average weight of most Americans on the rise, the rate of OSA also has likely risen since being overweight is one of several risk factors for developing OSA.
What are common risk factors for OSA?
In adults, the most common risk factors for OSA include:
- Being overweight (however – people who are NOT overweight also can develop OSA);
- Large neck size (circumference);
- Having large tonsils, a large tongue or other mouth and throat issues that reduce the size of the upper airway;
- Being a middle-aged or older man;
- Being a post-menopausal woman;
- Being a smoker.
How can a person get diagnosed?
If you have any of the symptoms of OSA, or you simply have one or more of the risk factors for OSA, talk to your health care provider. He or she can determine the best way to have you diagnosed and, if needed, treated for OSA. Advancements in technology allow for simpler and more cost-effective screenings than those used in the past.
What are the treatments for OSA?
OSA is a highly treatable disorder and weight loss in those with an elevated BMI can be effective. Achieving a healthier BMI also affords other benefits such as lowering risk of developing type 2 diabetes and cardiovascular problems.
Other OSA treatments range from dental devices and continuous positive airway pressure (CPAP) to surgery to correct mouth and throat abnormalities that interfere with breathing. (Your health care provider can determine which screening and treatment options are best for you)
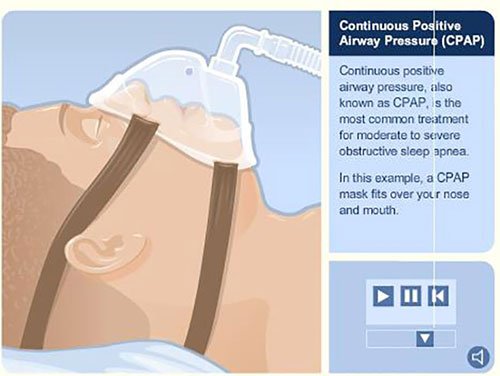
Image: National Heart, Lung and Blood Institute
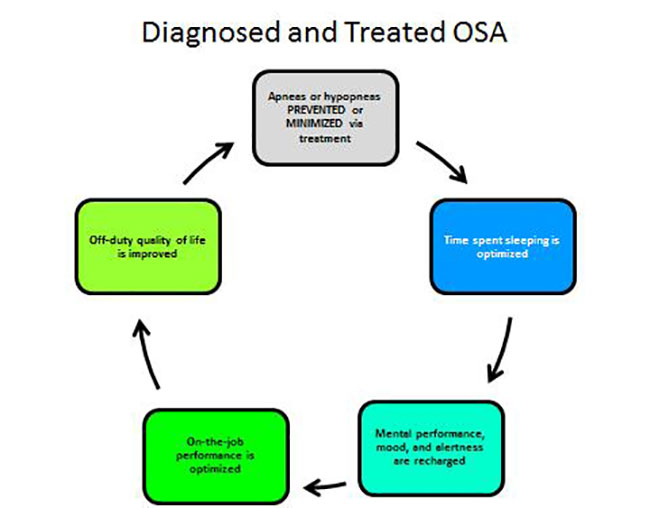
What are the benefits of treatment?
People with OSA experience the benefits of treatment almost immediately, and sometimes the benefits can be profound: after treatment, people with OSA sometimes report that they have not felt that alert in years. All functions that depend on sufficient recuperative sleep improve as well; mental sharpness returns and mood improves. Both of these benefit your on-the-job performance and your home life. Your overall health and wellness also improve, including lowered blood pressure, improvement in functions that, in turn, decrease your risk of type 2 diabetes, improvement in functions that reduce your risk of cardiovascular events and cardiovascular disease, and more.
Take-home
As a member of the FAA’s top-performing and highly motivated workforce, you owe it to yourself (and others) to remain at the top of your game by keeping yourself healthy. Being screened for OSA is a big step in that direction and ensuring that the FAA remains the safest and most efficient airspace system in the world.
Stay Fully Charged and ahead of OSA by learning more about the signs and symptoms, diagnosis, and treatment options for OSA. The National Heart, Lung and Blood Institute offers information on OSA and other sleep problems. Please visit the National Institute of Health’s website to learn more about OSA and see your healthcare provider soon.

